
It’s Eating Disorders Awareness Week, and it’s about time we tackled some core misconceptions
Too many people are still not seeking or receiving help for eating disorders in the UK. Charities such as Beat and AnorexiaBulimiaCare estimate more than 2.75 million people may be missing from the official figures owing to a lack of awareness. Now, during Eating Disorder Awareness Week, it’s time to join the conversation and speak out against common misconceptions.
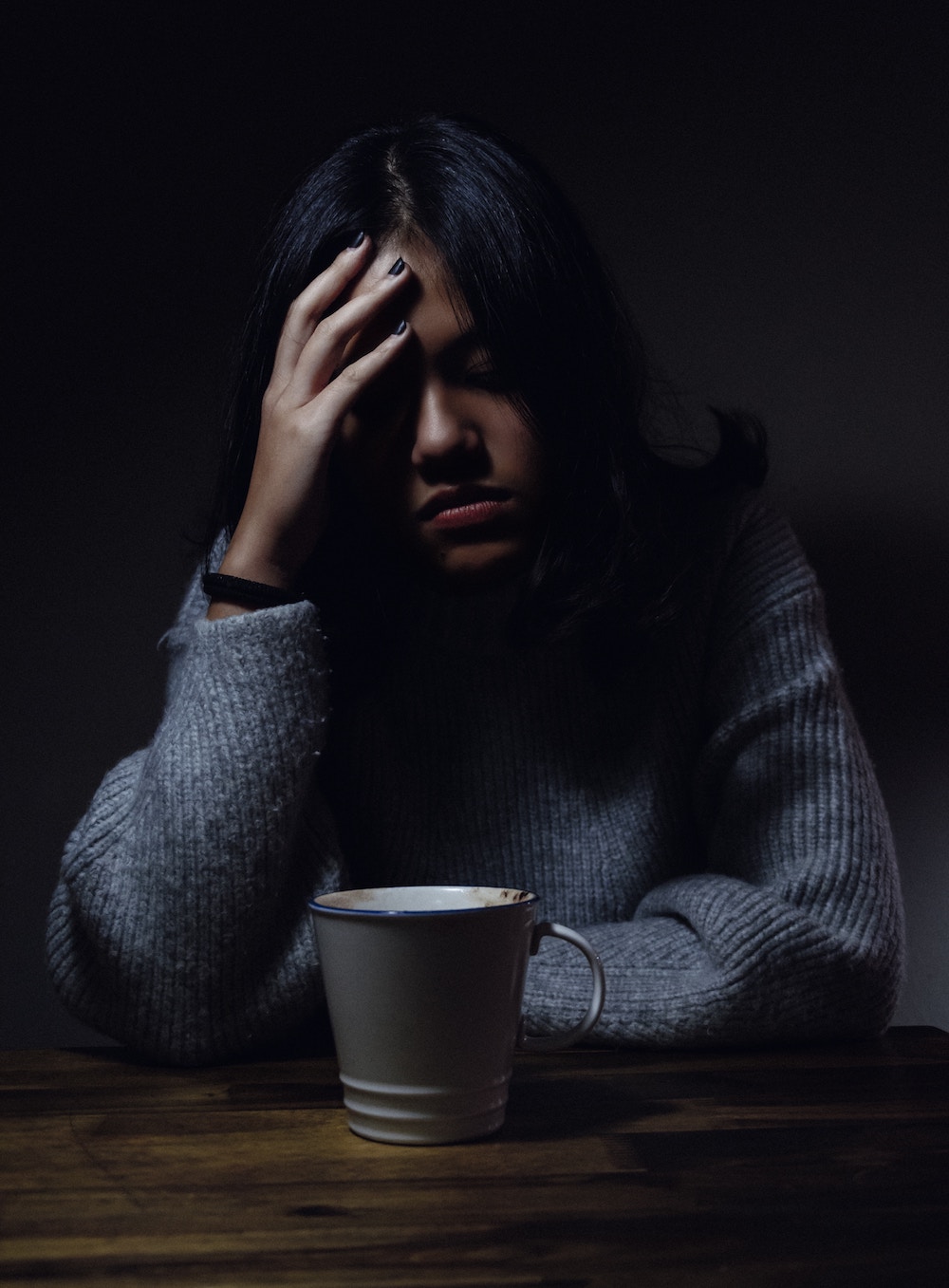
One of the hardest things for a sufferer to do is to recognise and accept that they have a problem. With such stringent medical diagnostics and a lack of societal awareness, many sufferers end up feeling like they are simply “causing a problem”. Mental illnesses are not a lifestyle choice, but a serious health condition, and can distort an individual’s thoughts and emotions.
Ironically, eating disorders often have very little to do with food – food is just the expressive tool. For many, their eating disorder is providing a sense of control and stability that is not found elsewhere. By focusing attention towards food, a sufferer can be avoiding, numbing, or even blocking an underlying painful feeling or emotion.
One of the most harmful misconceptions is that too many people still think one must look skeletal in appearance to have an eating disorder. In reality, weight is not an easy means to detect an eating disorder. Sufferers can be all shapes and can experience fluctuations in weight and therefore it is important not to judge someone just by looking at them.
Often, the negative thoughts penetrate so far into the sufferers’ mind that they can become increasingly isolated from friends and family. Those they are closest to can develop a sense of guilt and the perception that the disorder may have arisen in that person because of them – but this is not necessarily true.
Eating disorder thoughts are prevalent almost every minute of the day. Every decision can be influenced by how much energy could be consumed or expelled, and whether food will be present. As such, while meal times can be particularly difficult, simple things such as shopping, socialising with friends, or attending a work meeting can also be hard.
Writing a food plan is one thing, sticking to it is another. In many cases, those who are suffering from an eating disorder will need counselling and professional support in addition to meal planning.

As all eating disorders have personalised traits, there is a large variation between what can be considered “safe” foods, that they are comfortable eating, than many people expect. It is important not to comment “with surprise” on what a sufferer is eating, as this may exacerbate guilt.
As mentioned earlier, sufferers can be any size, and therefore the most significant health risks will depend on the individual eating disorder classification. Sufferers can experience deterioration in skin vitality, and poor hair and nail conditions. A large area of concern can be around the decline in bone condition, as well as the excessive pressure that can be put on the heart.
The mental health foundation estimates that between 10–25% of sufferers are men. While prevalence rates are recorded higher in teenagers, Beat has identified children as young as six with anorexia, and adult diagnosis within 70-year-olds.
While it’s true that many sufferers do get better, they need to be in the right place to engage with recovery. Priory Group, the leading independent provider of behavioural care in the UK, advise that early intervention is increasingly being recognised as important: once thoughts turn into learned behaviours they can be even more difficult to change.
For more information and support, visit Beat

